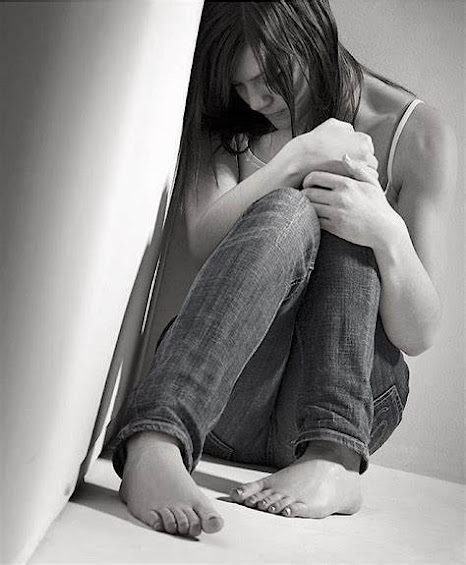
Depression
It's important to note that depression is a heterogeneous condition, meaning it can manifest differently in different individuals. The specific brain changes associated with depression can vary from person to person. Additionally, the relationship between brain changes and depression is complex and not fully understood.
Treatment for depression often involves a combination of psychotherapy, medication, lifestyle changes, and support from mental health professionals. The goal is to alleviate symptoms, promote healthy brain function, and improve overall well-being. Early intervention is important, as untreated depression can lead to more severe and long-lasting effects on the brain and mental health.
Depression is a complex mental health condition that can have significant effects on the brain. While the exact mechanisms underlying depression are still being studied, there are several ways in which depression can impact the brain:
1. Neurotransmitter Imbalance: One of the most widely accepted theories about depression involves a disruption in neurotransmitters, which are chemical messengers that transmit signals between brain cells (neurons). The most commonly implicated neurotransmitters in depression are serotonin, norepinephrine, and dopamine. A deficiency or imbalance in these neurotransmitters can affect mood regulation, leading to symptoms of depression.
2. Structural Changes: Chronic depression has been associated with structural changes in the brain. These changes can include a reduction in the size of certain brain regions, particularly the hippocampus, which plays a key role in memory and emotion regulation. It is believed that ongoing stress and the release of stress hormones like cortisol may contribute to the shrinkage of the hippocampus.
3. Functional Alterations: Depression can also affect the way the brain functions. Functional brain imaging studies, such as functional magnetic resonance imaging (fMRI), have shown that people with depression often exhibit altered patterns of brain activity, particularly in regions related to mood regulation and emotional processing. For example, the prefrontal cortex, which is involved in decision-making and emotional control, may show decreased activity in individuals with depression.
4. Neuroinflammation: There is growing evidence to suggest that inflammation in the brain, known as neuroinflammation, may play a role in depression. Some studies have found increased levels of inflammatory markers in people with depression. Chronic inflammation can disrupt normal brain function and contribute to depressive symptoms.
5. Neuroplasticity: Neuroplasticity refers to the brain's ability to reorganize and adapt. In depression, there may be disruptions in neuroplasticity, which can affect a person's ability to recover from the condition. Antidepressant treatments, such as psychotherapy and medication, aim to restore healthy neuroplasticity and help the brain adapt to more positive patterns of thinking and behavior.
6. Neurocognitive Impairments: Depression can also lead to cognitive impairments, such as difficulties with concentration, memory, and decision-making. These impairments can affect a person's daily functioning and quality of life.

It's important to note that depression is a heterogeneous condition, meaning it can manifest differently in different individuals. The specific brain changes associated with depression can vary from person to person. Additionally, the relationship between brain changes and depression is complex and not fully understood.

Treatment for depression often involves a combination of psychotherapy, medication, lifestyle changes, and support from mental health professionals. The goal is to alleviate symptoms, promote healthy brain function, and improve overall well-being. Early intervention is important, as untreated depression can lead to more severe and long-lasting effects on the brain and mental health.


No comments:
Post a Comment